Click To Listen To PodCast Here PNAS: Welcome to Science Sessions. I’m Paul Gabrielsen. The Aedes aegypti mosquito carries malaria, dengue fever, yellow fever, chikungunya, and Zika. But there may be a way to eliminate this and other harmful invasive species, through an application of gene editing called a gene drive. A gene drive encodes both a gene edit and the ability to copy that edit so that the next generation is guaranteed to inherit it and the edit rapidly spreads through the population. Kevin Esvelt of the Massachusetts Institute of Technology proposed that the CRISPR/Cas9 gene editing system, first announced in 2013, could be the engine behind a gene drive. Soon after the proposal, however, Esvelt and others expressed concerns about the effect of such a self-propagating gene drive on ecosystems. In a recent PNAS paper, Omar Akbari of the University of California, San Diego and colleagues presented what could be a safer form of a gene drive. They developed a method of encoding only part of a gene editing system into the Aedes mosquito. Akbari’s results could lead to a gene drive that achieves the goal of controlling harmful species but carries less risk for unintended and uncontrolled effects on native populations of those same species. Esvelt begins by telling the story of his gene drive proposal. He was among the first to experiment with the CRISPR/Cas9 system, but almost left the field as CRISPR’s popularity skyrocketed. One morning, his outlook changed. Esvelt: I was walking to work through the Emerald Necklace in Boston, and there was actually a turtle in the water that day, which was a rare spotting. And I was just wondering, are we ever going to edit any of these organisms? In the wild, I mean. And I concluded, well probably not just because whenever we make a change it's for our benefit not that of the organism, and so natural selection tends to wipe the floor with them. So then I wondered, but wait, what would happen if you encoded the CRISPR system that you used to make a genome edit adjacent to the change you're going to make? Then when it mated with a wild organism, the offspring would inherit your change and the instructions for making it, and it would then edit the original version from the other parent to have your new edit. And then, that would ensure inheritance by the next generation and the next and the next and the next. PNAS: Esvelt’s musings led to the gene drive proposal. Others had proposed similar systems, going back even to the 1940s. But now with CRISPR, the idea of a gene drive could become reality. Esvelt: So the first day was pretty much total excitement and elation at all these possibilities because this could be the key to eradicating malaria, schistosomiasis, all sorts of other diseases. The second day all of my doubts kicked in, thinking about - isn't this going to cause problems if it keeps on spreading, as presumably it would? How are we going to ensure that it's safe? You can't really test it in the field safely because it would probably just take off, so how do you run a field trial? Is an isolated island enough? What if it gets off? PNAS: In 2017, Esvelt and colleagues wrote that gene drives could spread remarkably quickly through an invasive animal population, but carry a significant risk of spreading to native populations as well. That risk warrants extreme caution in field trials and more research into safer forms of the technology. This is where Akbari comes in. In the CRISPR system, the protein Cas9 acts as the scissors, cutting DNA at a location specified by a strand of guide RNA. Akbari and his colleagues encoded the gene for the Cas9 protein into the Aedes mosquito genome. Akbari: Without the presence of the guide RNA, the Cas9 essentially doesn't cut. So, it's off. To turn it on, one would need to either inject the guide RNA into the organism or genetically cross the Cas9-expressing strain to other strains that express guide RNAs. PNAS: Akbari and colleagues have already employed the Cas9 embedded in the mosquitos’ genome to manipulate eye and body color, among other edits. If employed in a gene drive, Akbari’s partially-encoded system would be called a split gene drive. Akbari: So the split drive approach, it's a self-limiting approach. So, it essentially can't spread on its own; you would need to continually supply the Cas9 into the population. So, this type of drive is safe in that it can't spread on its own. The split gene drive approach is a good approach for studying and engineering and designing them in the laboratory and understanding how effective they spread in the presence of Cas9. It could be used in the field as a self-limiting-type approach and I think it would work, but again it would also require significant effort in terms of inundating the population with these gene drive-containing organisms and given that property, it makes it less attractive than a full drive that could actually spread itself. PNAS: Esvelt says that although Akbari’s work can be viewed in the context of a gene drive, it also fulfills one of the basic promises of CRISPR: to accelerate fundamental research. Esvelt: So the main impact of this paper, which is very well done, is to create tools that will make genome engineering in these mosquitoes fantastically easier. PNAS: Esvelt’s vision of the way forward for invasive and harmful species control is to give communities and regions the tools they need for small-scale ecological engineering. Esvelt: For almost all potential applications we need to focus on building local drive systems, that is, constructs that will alter a wild population, but only locally. That is, they cannot spread indefinitely. Just because it is hard to see how you're going to get more than 100 countries to agree, even on something like getting rid of these invasive mosquitoes that spread dengue and chikungunya and Zika and yellow fever. Thank you for listening. Find more Science Sessions podcasts at pnas.org/multimedia. Link to website
1 Comment
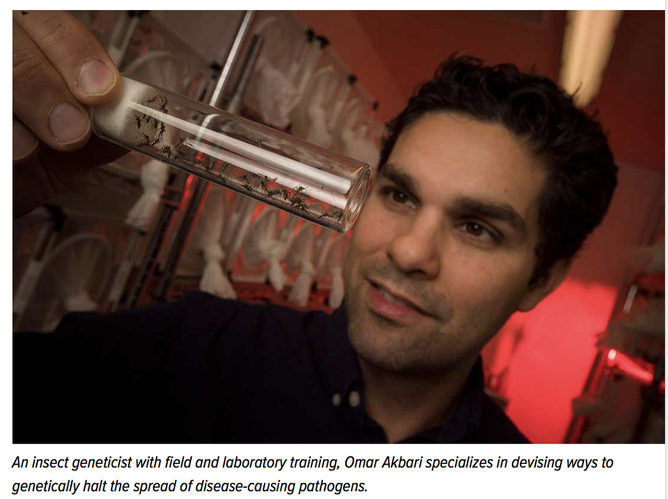
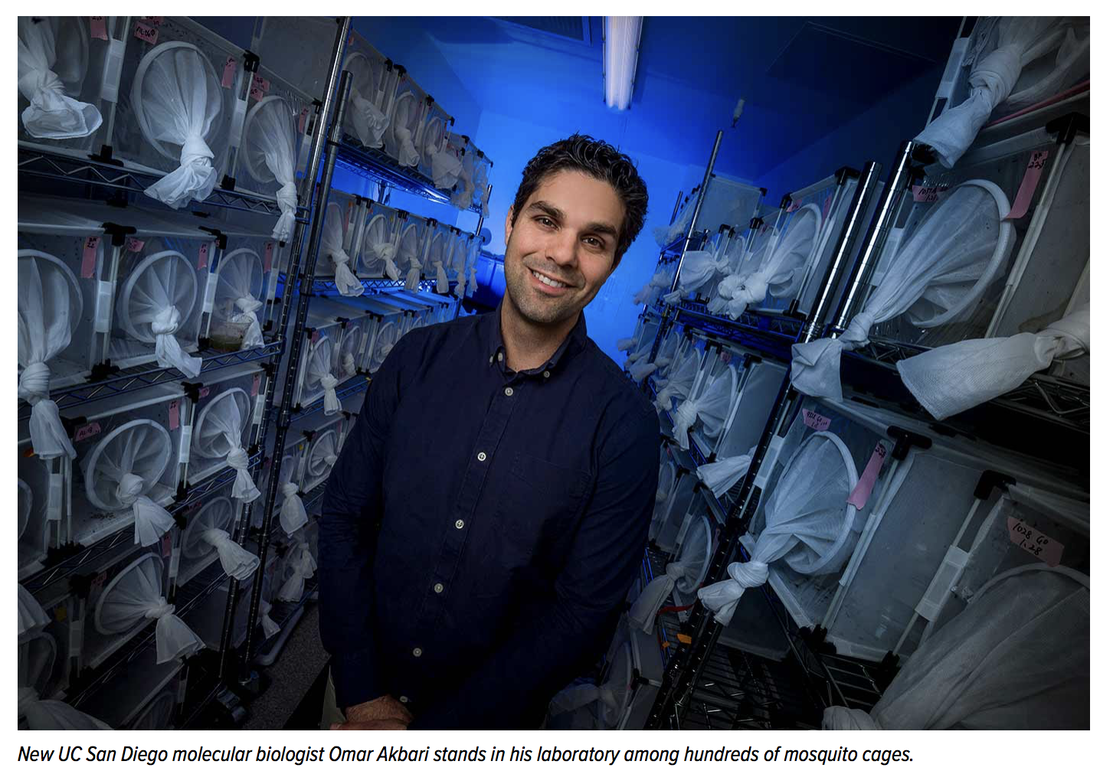 Link to Article by Mario C. Aguilera Enter Omar Akbari’s insect zoo and it’s immediately clear that you’ve entered a different world. It’s not that you’ve passed through several layers of containment that keep the bugs securely locked away… nor the fact that the temperature has just escalated 20 degrees… nor that the room is kept at 60 percent humidity—just the way mosquitoes like it. Rather, what becomes immediately apparent is Akbari’s unmistakable affinity for the pests and an ability of knowing just about everything there is to know about them. Having just arrived on the UC San Diego campus as a faculty member in the Division of Biological Sciences, Akbari comes armed with a unique skill set aimed squarely at disease-carrying insects and the potential to revolutionize how we fight them. Just as canine experts can unmistakably identify this Lhasa Apso and that Shih Tzu, and how to breed each, Akbari’s mosquito expertise affords him uncanny perspectives on how to stop mosquitoes from spreading disease. New UC San Diego molecular biologist Omar Akbari stands in his laboratory among hundreds of mosquito cages. With a quick glance inside one of the stacked cages in his lab, Akbari deftly identifies a mosquito’s species… its sex… mating habits…. feeding regimen… and what a mosquito is doing at any given moment. To the casual observer, it might appear as a bunch of bugs sitting idly around a cage. But through Akbari’s lens, this scenario is much more. Years of getting to know these blood-lusting creatures tells Akbari that these males are passionately waiting for the opportune moment a female is ready to mate, a situation accelerated when Akbari kick starts the mating ritual with a quick blast of air to get things stirred up. He can carefully describe the process through which a mosquito pierces human skin and extracts blood, and with it the potential of transmitting pathogens. And he explains all of this while a hungry mosquito is feeding off of his blood. For the love of mosquitosOmar Akbari’s story doesn’t trace the typical narrative of an emerging biologist. No early attraction to science. No stories of youthful adventures as a backyard wilderness explorer. Shockingly, not even a bug-collecting kit. His story starts in the placid town of Idaho Springs, Colorado. Set in the mountains an hour’s drive from Denver, Akbari grew up the proud son of the owner of the town’s only movie theater. His passion for science began to blossom in high school but didn’t shift gears until he attended the University of Nevada, Reno, where he took a job in a lab that exposed him to the wonders of science. “I started reading scientific papers and quickly began to love science,” said Akbari, who speaks in deceptively hushed tones but gradually ensnares his audience with the confidence that they are listening to someone who has clearly found his passion and purpose in life. “The ability to explore questions was really interesting to me. The idea that you could actually solve real-world problems became what I’m most interested in—the ability to save lives.” During his four summers in Reno earning combined bachelor’s and master’s degrees, he found a job that taught him all there is to know about eradicating pathogen-carrying bugs, known as “vector control.” He recalls the thrill of going into the field and bringing back mosquitoes to test for West Nile virus and other pathogens. “I learned how mosquitoes are controlled but I also learned about the cost and environmental impact, which was shocking and ridiculous,” said Akbari, who also obtained his Ph.D. at Nevada-Reno. “Having first-hand exposure to vector control and seeing the chemicals, oils and insecticides that were in use—I found that to be a major problem. I feel like that motivated me to try and invent a solution.” During his next stop at a postdoctoral position at the prestigious California Institute of Technology, Akbari’s relationship with mosquitoes deepened. His seven-year stay in Caltech Professor Bruce Hay’s lab provided an unusual level of expertise, along with a lasting bond with the insects. “Omar is one of the most talented, hardworking and imaginative young people I have seen,” said Hay. “He and UC San Diego are going to do great things together.” “I was at work all the time and basically lived with the mosquitoes,” he said. “I learned how to rear them. But I also learned from them. If you look at the number of mosquitoes we have in our lab today, you’ll see that we’ve optimized the process of raising them for research. No other lab has this many different strains. (My lab) has become really good at it, and it’s because I lived with them and worked with them so closely.” Know thy enemy Globally, more than three billion people are at risk of infection from malaria, which causes some 450,000 deaths per year and takes a child’s life every two minutes. For Akbari, these statistics are of interest personally as well as professionally. With two kids of his own at home, he openly wonders about how he would feel if one of his own was bitten by a mosquito and became infected. Even with a clear affinity for mosquitoes, Akbari is quick to point out that they are perhaps the most dangerous animals in the world. His specialty is the species Aedes aegypti, also known as the “yellow fever mosquito,” which can also spread Zika, dengue and chikungunya—diseases with no effective vaccines. Akbari and the nine members of his lab are on a mission to invent genetics tools and technologies that control the spread of disease and prevent pathogen transmission. They look to devise ways of driving laboratory-engineered genes—which disrupt normal pathogen inheritance pathways—into wild mosquito populations. Of late, Akbari is excited about prospects of a new weapon. He’s attempting to create genetically sterile mosquito males, which mate with wild females and pass the genes to their offspring. The eggs hatch and die as larvae. “You are releasing males that mate and produce no viable offspring,” said Akbari. “Over time that suppresses specific populations. This has been shown to significantly reduce specific insect populations.” The concept has been proven in fruit flies and Akbari is giddy at the prospects of trying the method in mosquitoes that carry pathogens. “(Akbari) is always full of so many ideas and I think many of us in his lab are amazed at how he comes up with them,” said Anna Buchman, a researcher who has known Akbari for more than 10 years and worked in his lab for the past three. “For example, we are working on Zika-resistant mosquitoes. Omar just gets ideas and says, ‘Let’s just try this.’ A lot of those types of projects actually start to become big things but started in a minor direction.” With such non-traditional approaches to solving mosquito disease transmission, Akbari will be working alongside researchers in the campus’ new Tata Institute for Genetics and Society in using UC San Diego-developed genetics technologies to eradicate malaria in India, as well as agricultural and health-related applications. As with the entire Tata Institute team, Akbari is committed to developing genetics tools for broad public benefit, and only introducing such advancements under safe and ethical constraints. Akbari also comes to campus as the leader of a $15 million Defense Advanced Research Projects Agency (DARPA) project to investigate ways to genetically influence inheritance, or “gene drive,” to spread desired genes in wild populations and suppress harmful organisms. Other UC San Diego researchers are part of this Safe Genes research team investigating ways to combat disease-carrying mosquitoes in California. “For his generation, working in vector biology and insect molecular biology, he’s one of the best and brightest,” said UC Irvine’s Anthony James, Donald Bren Professor of Microbiology and Molecular Genetics and a renowned mosquito scientist. “I’m really happy that there’s somebody of his caliber working on the Aedes aegypti species because they are a big deal. I view him as one of the two or three people worldwide who are doing excellent work on that species.” ‘One success can change the world’Getting to know the “mosquito man” is getting to know someone who clearly values a deep work ethic, but also collegiality and family life. Deflecting the “I” of his work into the collective “we” is a noticeable aspect of his ethos to highlight his team’s unified efforts. “The work that we’re doing in the lab and the ideas (Akbari) has are the future of genetic modification,” said Buchman. “I think we are going to see him really contribute in a very significant way to this field. As his career develops he is going to be a person that’s known.” You’ll see Akbari playing pickup basketball on campus with the same skill and subtle ferocity seen in his research. His lab members will tell you that he no longer spends all day and night with his precious mosquitoes—although he still pours more time and passion into his work than most. These days he promptly gets home to spend ample time with his 6- and 2-year-old daughters and doing the things that dads do (yes, including singing Frozen songs together). “Many of the projects we work on bridge the borderline of impossible,” said Akbari. “We tend to have far more failures than successes. Constant failure can be very difficult and frustrating to deal with, but I always remind myself that given the scope of our projects, even one success can change the world.” Download Full PDF  Can gene drives end mosquito-borne disease? Infectious Disease News, February 2018When Omar S. Akbari, PhD, moved his lab of genetically modified mosquitoes from the University of California, Riverside, to the University of California, San Diego, he took only eggs, collecting some from each strain and sealing them in containers for the 90-mile trip south. “Just the eggs. Not the adults — that’s how they’d escape, if something were to happen,” Akbari, a biologist and assistant professor at UC-San Diego, told Infectious Disease News. Omar S. Akbari, PhD, biologist and assistant professor at the University of California, San Diego, said the world will have to decide if it wants to use gene drives. “I hope that we do,” he said.Akbari’s lab contains 260 cages filled with 130 strains of genetically modified mosquitoes plus additional cages for more experiments. The lab is designed to keep mosquitoes inside. Four doors separate the insectary from the outside world. Even if a mosquito were to escape from its cage, an air blower triggered by the innermost door should keep it from getting out of the room. For good measure, there are mosquito traps positioned from the insectary to the hallway outside the main lab. Even if they did somehow escape, Akbari said many of his mosquitoes could not survive in the wild. Some could not even survive in the lab. Using a technology that allows scientists to make desirable edits in an organism’s genetic material, his lab has engineered what he called “interesting mutants.” These included mosquitoes with three eyes, three mouth parts, no wings, notched wings, eyes that were white instead of black and tiny eyes that presumably rendered the insects blind. This was not mad science, Akbari said, because each of the experiments had an applied reason for driving certain genes into a population. For instance, a system that produced striking yellow mosquitoes could be used to optically sort the insects and release only males into the wild. The experiments were conducted using CRISPR-Cas9, a gene-editing mechanism that scientists can use to drive a self-destructive gene — like one that produces offspring that cannot survive — through a population of insects. In just a short time, CRISPR-Cas9 has made a world without mosquito-borne disease seem more possible. “I think it’s fair to say it surprised a lot of people with how well it works,” Anthony A. James, PhD, professor of microbiology and molecular genetics in the School of Medicine and professor of molecular biology and biochemistry in the Ayala School of Biological Sciences at UC-Irvine, said in an interview. Infectious Disease News spoke with several experts about the promise of using gene drive technology, including CRISPR-Cas9, as a tool for mosquito control and its potential to eradicate mosquito-borne diseases. ‘We need better tools’Mosquitoes kill millions of people worldwide each year. According to WHO, malaria infected at least 216 million people worldwide in 2016, killing 445,000, most of them children in Africa. The Zika virus epidemic has caused thousands of cases of microcephaly in infants, mainly in Brazil, which also experienced a large yellow fever outbreak last year that prompted mass vaccination campaigns and raised fears that the disease would spread to the country’s largest cities. About half the world’s population now lives in an area at risk for dengue, which can develop into a serious and sometimes fatal disease. The first indigenous outbreak of chikungunya in the Americas began in 2013, sickening millions of people, according to the Pan American Health Organization. Efforts to control these diseases have historically focused on using pesticides to rapidly reduce populations of mosquitoes, like the aerial spraying that took place around Miami in 2016 to kill Aedes aegyptimosquitoes that carry Zika. Officials urge people to protect themselves by using insect repellent, covering exposed skin, fixing broken window screens and removing standing water in their yards. For decades, scientists have been trying to develop better ways to combat mosquito-borne diseases. Previous methods seem primitive compared with gene drives, whose promise has grown since the introduction of CRISPR-Cas9, which has made the process more efficient and straightforward. “Years of using insecticides and pesticides have shown us that it’s not sustainable,” said James, who began exploring genetic solutions to mosquito-borne diseases in 1986. “We don’t want to continue to put tons of potentially toxic chemicals for off-target organisms into the field. If we have something that’s better and cleaner and highly specific to the target organism, why not use it? We need better tools that are better targeted. Even though this is a new technology that hasn’t been in the field yet, it’s got to be better than pesticides.” After years of research without results, gene drive technology has progressed rapidly in the last several years since the introduction of CRISPR-Cas9. The system is seen as being critical to the future of mosquito control and the eradication of mosquito-borne diseases, but no gene drive has ever been approved for use in the wild, and the technology represents just one of many new areas of exploration. “There is no silver bullet,” Marcelo Jacobs-Lorena, PhD, professor of molecular microbiology and immunology in the John Hopkins Bloomberg School of Public Health, said in an interview. “If a gene drive is approved and implemented, I don’t think it can, by itself, eliminate a disease. We have to combine all the resources we have. That’s the only way we will conquer malaria or any other disease.” CRISPR is a helpful acronym for clustered regularly interspaced short palindromic repeats, and Cas9 stands for CRISPR-associated protein 9. Using CRISPR technology, scientists can modify genomic sequences by cutting and editing targeted sections of DNA. CRISPR-Cas9 is not the first gene drive technology to be tested by experts, but it has produced the most encouraging results. “I personally don’t believe that any other gene drive mechanism will work,” Jacobs-Lorena said. Key findingsScientists are exploring other methods for mosquito control, including interventions that do not necessarily require a gene drive to implement. Marcelo Jacobs-LorenaRecently, the EPA approved the use of a strain of Wolbachia for mosquito control. Passed to females during mating, the bacterium ensures that offspring do not survive. It works in both A. aegypti and A. albopictus mosquitoes, which transmit Zika, dengue, chikungunya and yellow fever. But Wolbachia is not effective against the many species of Anopheles mosquitoes that carry the Plasmodiummalaria-causing parasite. Results from two studies conducted at the Johns Hopkins Malaria Research Institute and published in Science last year raised the possibility of using other genetic methods to control malaria. In one, researchers altered the gene activity of several strains of A. stephensi mosquitoes to boost their immunity to the P. falciparumparasite. They found the process also altered the insects’ mating preferences so that genetically modified males preferred unmodified wild females and wild males preferred genetically modified females. This helped spread the genetic modification to successive generations of mosquitoes — an unexpected finding. It took only five generations, or around 10 to 12 weeks, for the modification to dominate the population. The mosquitoes have maintained a high level of resistance to the parasite for more than 7 years. “Our discovery is very important because it’s proof that spreading the gene doesn’t have to be based on a genetic mechanism. It could be something that changes the behavior of the insect,” George Dimopoulos, PhD, professor of molecular microbiology and immunology at the Johns Hopkins Bloomberg School of Public Health, told Infectious Disease News. In another chance finding, Jacobs-Lorena and colleagues discovered a new strain of the Serratia bacterium engineered to kill the malaria parasite. The bacterium spreads efficiently, making it different from other mosquito-infecting bacteria. The strain, which was unexpectedly found in the insects’ ovaries, is transmitted easily from males to females during mating, then from females to 100% of their progeny, allowing it to move rapidly through mosquito populations. Bringing all of this together, a study published in the Proceedings of the National Academy of Sciences of the United States of America (PNAS) in 2015 showed for the first time how gene drives can be used to spread antimalarial genes into a vector population. The study was the result of a collaboration between James, who had published findings on malaria-resistant genes in 2012, and two researchers from UC-San Diego, Ethan Bier, PhD, and Valentino Gantz, PhD, whose 2015 study in Science demonstrated that CRISPR-Cas9 could be used to spread gene mutations in fruit flies. Together, they adapted the technology quickly as a gene drive in mosquitoes. In another milestone study published in PNAS in November 2017, Akbari and colleagues showed how they engineered Cas9 strains to be easily expressed through generations of A. aegypti mosquitoes in a set of experiments that produced the “mutants” in his lab. This is only one-half of what is called a split-gene drive. Akbari and colleagues are working on the other half, which involves crossing Cas9 strains with guide RNA that recognize DNA sequences and measuring the rates of inheritance. Using CRISPR gene-editing technology in mosquitoes is just one application that is being studied by scientists. Numerous breakthroughs in other areas have occurred over the course of just a few years. Last year, researchers from Harvard showed they could use CRISPR-Cas systems to encode a short movie into the DNA of bacteria, a method that could be used to store data within living cells. The quick succession of these results has made researchers optimistic about the technology’s future applications. “The day before the discovery of antibiotics, the mildest infectious disease was life-threatening. After that, they at least became treatable. There are these major jumps that occur in science and medicine that have a profound effect,” James said. “It’s some scientist somewhere doing something that no one pays attention to and it turns out it’s a big deal, like the CRISPR biology.” Regulatory barriersWhen the first gene drive is introduced in the wild — perhaps not for another 5 to 10 years, according to Dimopoulos — it is unlikely to happen in the U.S., where James said getting the appropriate regulatory bodies on the same page is too much of an obstacle. “You have to be in a country that has an integrated regulatory system where all interested parties have a vote and it’s really straightforward. The United States is still so fragmented,” he said. “The USDA, FDA, EPA, CDC — there’s no single body that has a member of each one of those [agencies] that can work together.” George DimopoulosStill, James said a framework is in place for how to introduce a gene drive system in the wild. Under a four-phase trial plan devised by a working group at WHO, researchers would have to demonstrate that a gene drive is safe and effective. The next two phases would involve studies using large outdoor cages or the release of mosquitoes restricted to a certain geographic area or ecosystem, then an epidemiologic study showing that the drive has an impact on a disease. If all the criteria are met, a fourth phase would involve making it part of a standard disease control program. James anticipates that the first mosquito gene drive in the wild will involve a small number of releases in a confined area. Researchers will monitor the insects over several seasons to determine the impact. But because no country has adopted guidelines that would specifically permit the release of a gene drive organism, he said it is too early to speculate where the first one might occur. “There are efforts to bring regulatory structures up to speed. And we’re happy with that,” James said. “We work in public health. We’re trying to save people from these diseases. We don’t want to be known for doing something catastrophically stupid. That kind of defeats the whole purpose.” Ethical questionsThere are other barriers to using gene drives in the wild, including ethical questions about changing an animal’s biology. The ethics of gene drives may be a matter of debate, but experts do not foresee them having serious ecological consequences, such as a drive jumping to another species or making mosquitoes a more competent vector for another pathogen — two concerns that have been raised. “This is science fiction,” Dimopoulos said. Still, to make gene drives a reality, Akbari said it would be important to demonstrate control over a system before a gene drive is released in the environment, to show that it can be reversed in case of any unintended consequences. According to him, this is easily done by designing another gene drive that can target the initial sequences. His lab was one of several in the University of California system that received $15 million in gene drive-related funding from the Defense Advanced Research Projects Agency (DARPA), an agency in the U.S. Department of Defense that invests in breakthrough technologies. Akbari said one of the stipulations of the DARPA funding is that the researchers explore how a gene drive can be reversed. “This is definitely something that DARPA is interested in, mainly because if the gene drives got into the wrong hands and someone were to try to drive something as some kind of weapon, then how would you counter that weapon?” Akbari said. “We need countermeasures. Having countermeasures is definitely a high priority.” Experts theorize that a gene drive could be used to make a species of mosquito extinct. Some see little reason not to eradicate a species like A. aegypti, an invasive insect in the Western Hemisphere that has evolved to become a human pest. But is it ethical? According to Sahotra Sarkar, PhD, professor of philosophy and integrative biology at the University of Texas, there may indeed be legitimate reasons to drive a species to extinction but not without first having a public discussion and developing policy guidelines. “Until that happens, it would be unwise to recommend gene drives to drive any species to extinction,” Sarkar said. According to Akbari, the science around gene drives is moving so fast that ethical questions about their use are likely going to be harder to address than scientific questions. Source: Steve Zylius/UCI Anthony A. James, PhD, professor and microbiologist at the University of California, Irvine, and colleagues showed for the first time how gene drives can be used to spread antimalarial genes into a vector population.“We will reach a point where there is a drive system that can spread and can block the vector competence of malaria or dengue and we’ll have to decide whether or not to use it. I hope that we do,” he said. Experts also said that engaging and educating the public will be a significant hurdle to eventually using gene drives in the wild — maybe the biggest one. There already have been examples of this, including a plan to release genetically modified mosquitoes in the Florida Keys that was initially voted down by residents but ultimately approved. Outdoor caged trials of the same mosquitoes, manufactured by the British company Oxitec, began in India last year. Dimopoulos said one of the concerns is that the public will blame the release of a gene drive in the wild for an unrelated disease outbreak. “We have to face that there is a huge resistance in the world for anything genetically modified. That is the biggest barrier,” Jacobs-Lorena said. “The advantage we have with mosquitoes is that the ultimate aim is to save lives.” ‘Scientists vs. evolution’Whether using gene drives will achieve the ultimate goal of eradicating a mosquito-borne disease is unclear, but some experts are betting on the technology. UC-San Diego is building a new 2,000-square-foot insectary that is 10 times the size of the one in Akbari’s current lab. When it is finished later this year, Akbari will share the insectary with Bier. The goal of a gene drive is to block a pathogen long enough that it is no longer carried by mosquitoes, humans or any other animals, Akbari said. After that, the question is whether nature will cooperate. “I do think that evolution probably will find a way,” he said. “But given that we can engineer gene drives pretty fast, it would be an arms race: scientists vs. evolution.” Dimopoulos said there is chance that something better than CRISPR-Cas9 will be discovered and make it even easier to alter the genes of mosquitoes on a large scale. “It reminds me a little bit of when they sequenced the human genome,” he said. “If you would have told anyone 3 years earlier that they were going to [do that], no one would have believed you. People would have been laughing. Then, all of a sudden, there it was.” – by Gerard Gallagher References:
Download PDF Here |
Archives
June 2024
|
 RSS Feed
RSS Feed
